State Targeted Response Summary
Nevada's Response to the Opioid Crisis
Press Releases
DEPARTMENT OF HEALTH AND HUMAN SERVICES – DIRECTOR’S OFFICE
- 4126 Technology Way, Suite 100
- Carson City, Nevada 89706
- Telephone (775) 684-4000 · Fax (775) 684-4010
FOR IMMEDIATE RELEASE
DATE: Tuesday, May 01, 2018
CONTACT: Chrystal C. Main, Public Information Officer – (775) 684-4024; ccmain@dhhs.nv.us
Nevada Division of Public and Behavioral Health
Selects Awardees for Opioid Treatment And Recovery Centers Centers will provide integrated care
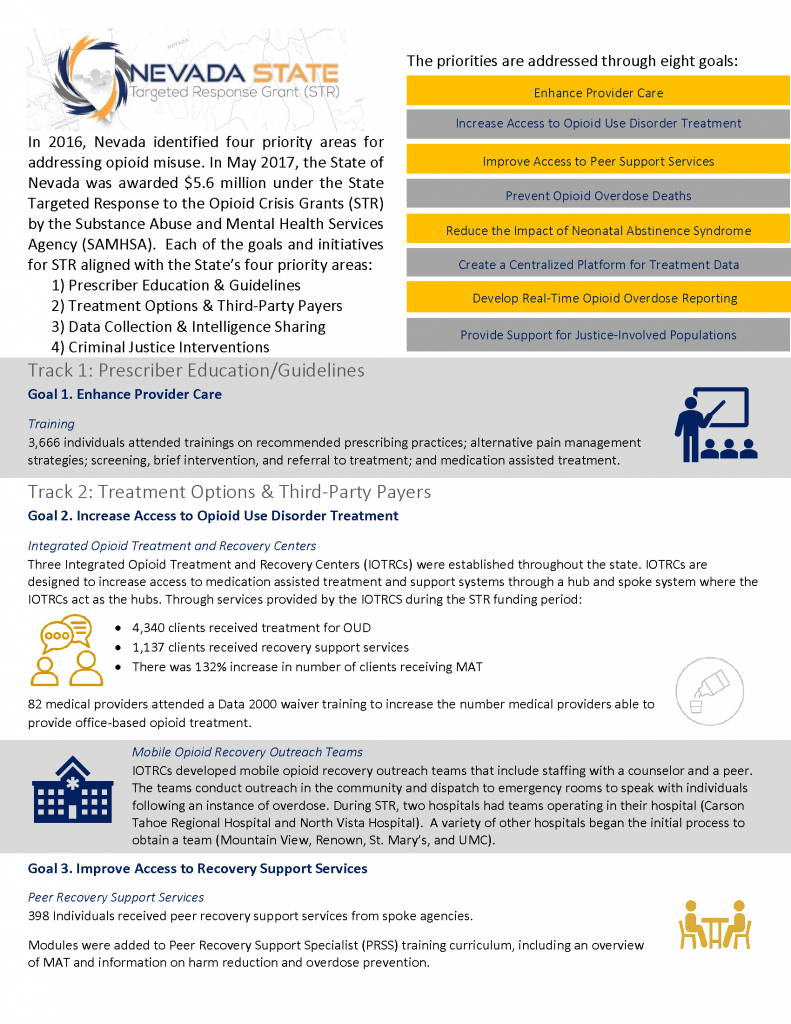
Carson City, NV — Richard Whitley, Director of the Nevada Department of Health and Human Services (DHHS) recently announced the names of three community provider organizations selected to receive the Opioid State Targeted Response (STR) Integrated Opioid Treatment and Recovery Centers (IOTRC) grants. “Improved access to services is key to combating the opioid crisis,” said Whitley. “By having treatment options, citizens may be able to return to the workforce as productive members of society.”
“Approximately 2.1 million dollars of the STR budget will go towards the IOTRC’s,” said Dr. Stephanie Woodard, Senior Advisor on Behavioral Health for the State of Nevada Department of Health and Human Services, Division of Public and Behavioral Health Bureau of Behavioral Health, Prevention, and Wellness. “The development of the IOTRC’s is an essential step in Nevada turning the tide on the public health crisis caused by the opioid epidemic. The Integrated Opioid Treatment and Recovery Centers will be funded for a six month project to expand access to high quality treatment and recovery services for adolescents and adults who are struggling with addiction to opioids. Despite having some of the best treatments available for opioid use disorder, we still have challenges linking people to care. The IOTRC’s are designed to connect those needing treatment to comprehensive care.”
IOTRC’s will provide integrated primary and behavioral health care for adults and adolescents with Opioid Use Disorder. They are designed to provide comprehensive, individualized evaluations of treatment needs and ensure that people presenting for treatment access appropriate care. For many people with opioid addiction the most effective treatment is the combination of counseling and Medication Assisted Treatment (MAT) with medications such as naltrexone, methadone, or buprenorphine. The IOTRC’s will provide a range of services and supports including MAT, care coordination, counseling, assistance with accessing community resources, and support for long-term recovery.
IOTRC’s serve as the center for care coordination within their formal network of care providers. These formal networks include intensive services, such as withdrawal management and residential services for people with the most severe treatment needs, as well as prevention and whole-health services, such as primary care and HIV testing. The Integrated Opioid Treatment and Recovery Centers will also have mobile recovery outreach teams to provide support and engagement in services following an overdose. To prevent fatal overdoses, IOTRC’s will also distribute naloxone, the antidote for opioid overdose, to individuals in the community who are at-risk for experiencing an opioid related overdose. The mobile recovery outreach teams will include peer supporters who have lived experience dealing with addiction. As subject matter experts in opioid use disorder treatment, the IOTRC’s will serve as regional consultants on addiction prevention, treatment, and recovery.
“Opioid STR funding is limited to two years. Our efforts to build a sustainable treatment and recovery system of care means these centers will also be required to meet specific certification criteria to receive the IOTRC’s designation. President Trump’s declaration of a public health emergency is also allowing states to apply for 1115 demonstration waivers to cover services, such as residential care for addiction. The Division of Heath Care Financing and Policy, Nevada Medicaid, is actively evaluating the financing models to sustain the IOTRC’s system of care.