Communities play a crucial role in addressing the opioid epidemic by implementing various strategies to prevent substance abuse, provide support and treatment for individuals struggling with addiction, and reduce the stigma surrounding addiction.

Websites
SAMHSA’s National Helpline
SAMHSA's National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish). Call 1-800-662-HELP (4357) or visit the website.
988 Suicide & Crisis Lifeline – Call. Text. Chat.
The 988 Lifeline provides 24/7, free and confidential support for people in distress, prevention and crisis resources for you or your loved ones, and best practices for professionals in the United States.
Behavioral Health Nevada
This website is a database of behavioral health providers in Nevada specializing in substance use disorder and co-occurring mental health disorder treatment services. All agencies listed are Certified by the Division, SAPTA (Substance Abuse Prevention and Treatment Agency).
National Institute of Drug Abuse (NIDA)
Information on how drugs affect the brain and body for teens, teachers, and parents.
Stop Overdose
To address the increasing number of overdose deaths related to both prescription opioids and illicit drugs, the Centers for Disease Control and Prevention (CDC) created a website to educate people who use drugs about the dangers of illicitly manufactured fentanyl, the risks and consequences of mixing drugs, the lifesaving power of naloxone, and the importance of reducing stigma around recovery and treatment options.
Tools & Resources
Opioid Epidemic Response: Employer Toolkit
Substance use and substance use disorder affects employees, workplaces, families, and communities. Employers have the opportunity to identify early signs and symptoms of a substance use disorder, and help connect employees to treatment and recovery supports. This toolkit developed by the Minnesota Department of Health includes five steps to prevent and address substance use disorder within your workplace.
How to Become an Overdose Reversal Medication Distribution Site in Nevada
Request to become an Overdose Reversal Medication Distribution site.
Nevada Fentanyl Test Strip Distribution Sites
A list and map of Fentanyl Test Strip Distribution Sites in Nevada.
Nevada Overdose Reversal Medication Finder
Find naloxone and overdose reversal medications in Nevada.
Behavioral Health Nevada
This website is a database of behavioral health providers in Nevada specializing in substance use disorder and co-occurring mental health disorder treatment services. All agencies listed are Certified by the Division, SAPTA (Substance Abuse Prevention and Treatment Agency).
How to Use Fentanyl Test Strips
Infographics and step-by-step instructions.
Establishing Peer Support Services for Overdose Response: A Toolkit for Health Departments
Peer support services (PSS) are a valuable component of a growing number of overdose response and linkage to care initiatives that can be implemented and supported by local and state health departments. This toolkit is for local and state health departments and community partners who are exploring opportunities to implement or enhance PSS within overdose response and linkage to care initiatives. This toolkit provides information, resources, tools, actionable steps and real-world examples informed by the latest research, subject matter experts and experiences from diverse settings across the country.
Screening Tools
Native Harm Reduction Toolkit
This toolkit was imagined and created by Arlene Brown, member of the Bishop Paiute Tribe, with support from NHRC staff, including Jessica Smith. It has been informed by Tribal and Urban Native people from across California and brings together resources from Indigenous harm reduction leaders from across the country and beyond.
Spirit of Harm Reduction: A Toolkit for Communities of Faith Facing Overdose
A toolkit addressing faith and faith leadership in engaging with people who use drugs and harm reduction practices.
PACT Coalition
The PACT Coalition seeks to empower Southern Nevada with the resources to prevent substance misuse for all ages and promote recovery through culturally competent advocacy, education, stigma reduction, support, and outreach. A diverse cross-section of community leadership is represented by the PACT Coalition that will work together to ensure a sustainable future and a healthier community. PACT Coalition keeps an updated resource list for Southern Nevada.
Engaging Community Coalitions to Decrease Opioid Overdose Deaths Practice Guide 2023
This guide was developed in recognition of the need to center community engagement throughout the efforts to address the opioid overdose crisis. This guide exists to help communities decrease opioid overdose deaths; it includes tools and real-world examples that can be used to build and strengthen community coalitions that work to reduce opioid overdose deaths.
Overdose Reversal Medication for Community Organizations
This guide includes Naloxone Distribution in Nevada guidelines and best practices for community based organizations.
The Rural Community Toolbox
This website includes resources to address substance use disorder (SUD) and the opioid crisis, as well as Federal resources that can help rural communities become strong, healthy, prosperous, and a resilient place to live and work.
Know Your Pain Meds
Provides information on how opioids work, alternatives to pain medicine, the overdose reversal medication naloxone, a substance use disorder treatment finder, and submit concerns you have about a medical provider.
Overdose Prevention and Response Toolkit
This toolkit provides guidance to a wide range of individuals on preventing and responding to an overdose. The toolkit also emphasizes that harm reduction and access to treatment are essential aspects of overdose prevention.
Storage and Disposal of Medication
Improper prescription drug use is a serious public health issue. Storing and disposing of medications properly can help reduce harm.
Posters & Infographics

Opioid Trifold Brochures
Opioid Information Brochures for Providers or Consumers help educate on opioids and opioid use, including effects of opioid use, pregnancy and opioid use, medications for opioid use including opioid overdose reversal medications, and treatment options for persons using opioids.
Download or request free hard copies

Stimulant Trifold Brochures
Stimulant Information Brochures for Providers or Consumers help educate on stimulants, including the effects of stimulants use, pregnancy and stimulant use, and treatment options for persons using stimulants.
Download or request free hard copies
Opioid Use Disorder Treatment and Recovery Fact Sheet
This fact sheet contains important information about treatment and recovery of opioid use disorder for patients, families and friends.
Download the fact sheet
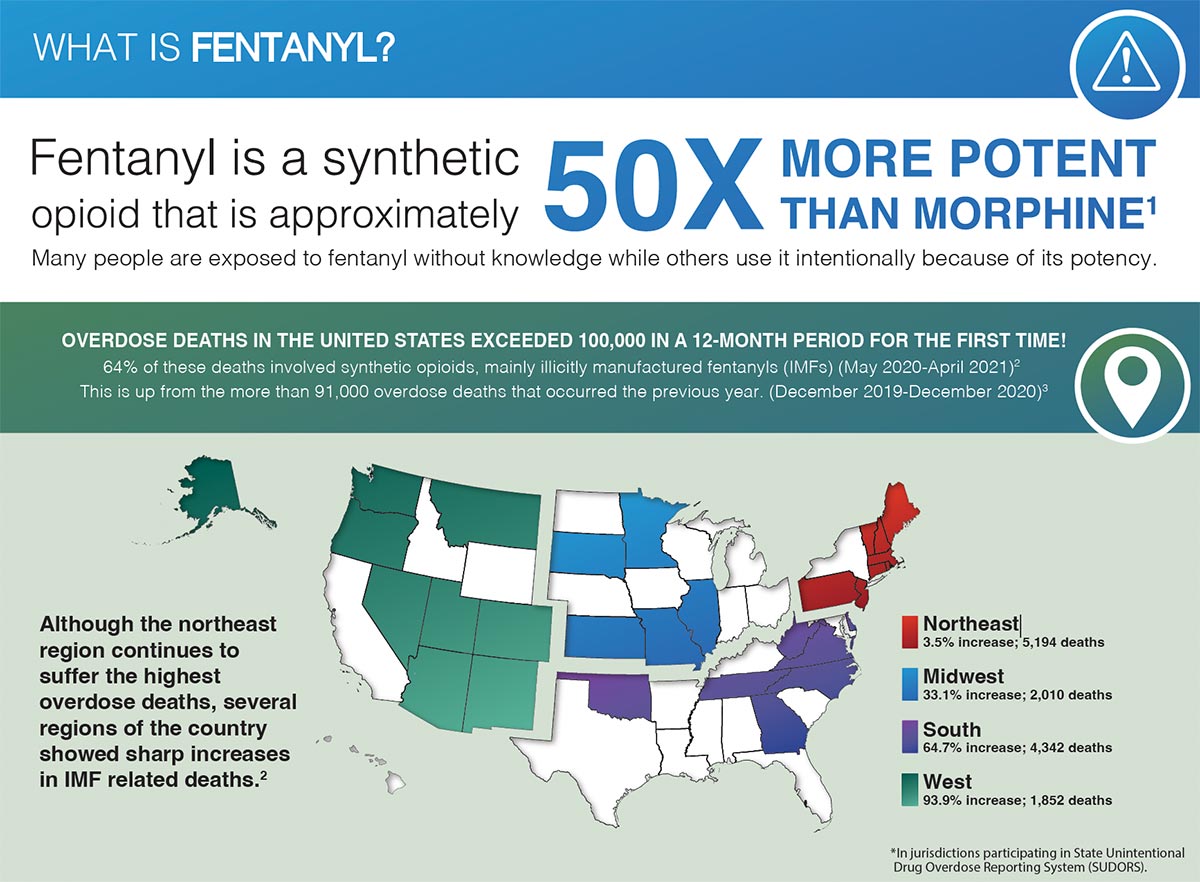
What is Fentanyl? Infographic
This infographic was developed by the National Institute on Drug Abuse.
Download the infographic
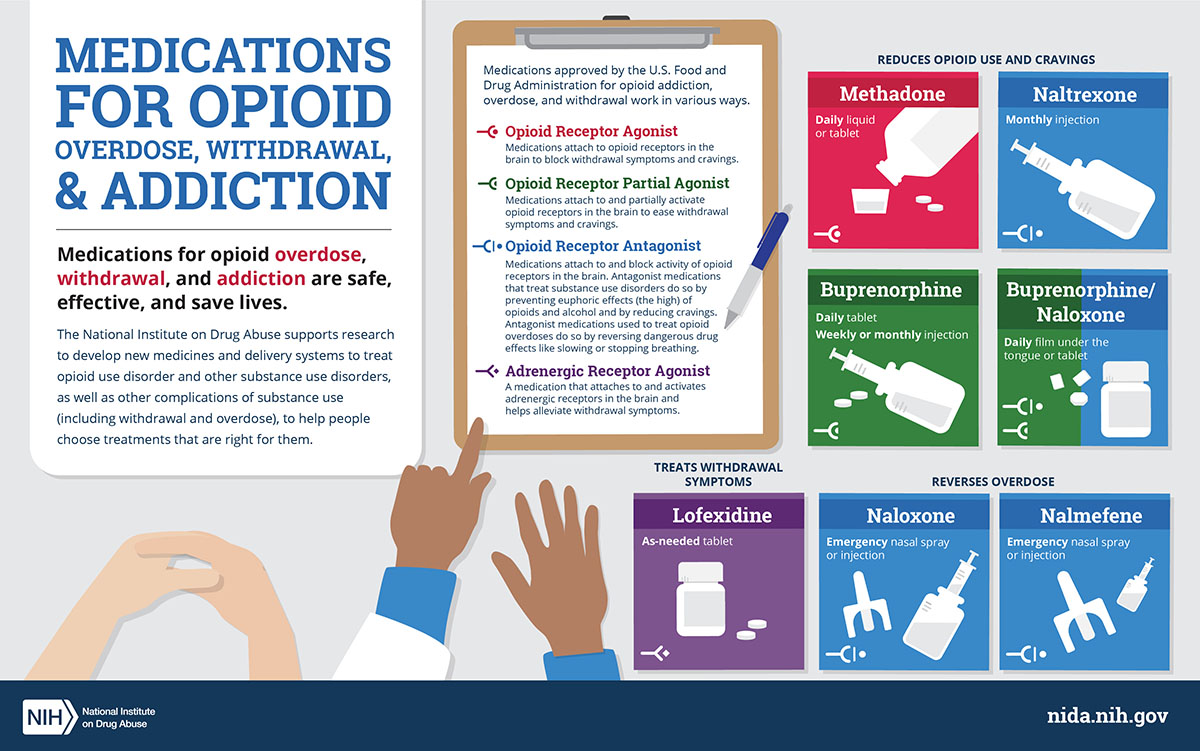
Medications for Opioid Use Disorder (MOUD) Infographic
This infographic shows different types of medications approved by the U.S. Food and Drug Administration for opioid overdose, withdrawal, and addiction.
Download the infographic
Are You Taking Medicine for Opioid Use Disorder and Are Pregnant or Thinking about Having a Baby?
This poster is for clients and their family members in OUD treatment who are pregnant or who are currently not pregnant but of childbearing age.
View the SAMHSA Poster
Publications
Xylazine Basics: Overdose Prevention, Harm Reduction, and Wound Care
This document provides information on xylazine, a non-opioid veterinary tranquilizer used as an additive in illicit drug supplies, notably in combination with heroin and fentanyl. It discusses the effects of xylazine use, including sedation and potential risks such as hypotension and bradycardia. The document also emphasizes harm reduction interventions for individuals who may encounter xylazine in the drug supply, including the use of naloxone for responding to overdoses and the importance of wound identification and treatment.
Dear Colleague Letter – Xylazine
This "Dear Colleague" letter from the Substance Abuse and Mental Health Services Administration (SAMHSA) provides a report on the risks of Xylazine.
Beyond Addiction: How Science and Kindness Help People Change
The most innovative leaders in progressive addiction treatment in the US offer a groundbreaking, science-based guide to helping loved ones overcome addiction problems and compulsive behaviors.
Evidence-Based Strategies for Preventing Opioid Overdose: What’s Working in the United States
There are strategies that can assist community leaders, local and regional organizers, non-profit groups, law enforcement, public health, and members of the public in understanding and navigating effective ways to prevent opioid overdose in their communities. Use this information as a reference for evidence-based practices that have been successfully implemented in the U.S.
In My Own Words
A compilation of essays by individuals supported by Medication-Assisted Treatment in long-term recovery.
Webinars & Online Learning
Current News & Research
DEA Reports Widespread Threat of Fentanyl Mixed with Xylazine
WASHINGTON - The U.S. Drug Enforcement Administration is warning the American public of a sharp increase in the trafficking of fentanyl mixed with xylazine. Xylazine, also known as “Tranq,” is a powerful sedative that the U.S. Food and Drug Administration has approved for veterinary use.
Southern Nevada Health District calls attention to xylazine risk
The Southern Nevada Health District (SNHD) is urging heightened public awareness of the health dangers associated with xylazine, an animal tranquilizer that is increasingly being found in the country’s illicit drug supply and linked to overdose deaths throughout the United States. Xylazine, also known as “tranq,” is not approved for human consumption. It can be life-threatening and is especially dangerous when combined with opioids such as fentanyl.
The Opioid Epidemic’s Toll on Children
This article from the Johns Hopkins Bloomberg School of Public Health discusses the opioid epidemics toll on children.
