Practitioners play a crucial role in helping individuals with opioid use disorder (OUD) by providing comprehensive care, support, and access to evidence-based treatments. Here are some useful resources for practitioners working with individuals with opioid use disorder (OUD).

Websites
Nevada Recovery Friendly Workplace
In an effort to improve Nevada’s workplaces, the State of Nevada has developed a Recovery-Friendly Workplace Program to reduce the stigma of substance use and encourage workplaces to support treatment and recovery. Through education, and policy and procedure development to support recovery in all aspects, the program provides free resources to become a designated recovery-friendly workplace.
988 Suicide & Crisis Lifeline – Call. Text. Chat.
The 988 Lifeline provides 24/7, free and confidential support for people in distress, prevention and crisis resources for you or your loved ones, and best practices for professionals in the United States.
Nevada Zero Suicide
The Zero Suicide framework is a system-wide, organizational commitment to safer suicide care in health and behavioral health care systems. The framework is based on the realization that suicidal individuals often fall through the cracks in a sometimes fragmented and distracted health care system. A systematic approach to quality improvement in these settings is both available and necessary.
Behavioral Health Nevada
This website is a database of behavioral health providers in Nevada specializing in substance use disorder and co-occurring mental health disorder treatment services. All agencies listed are Certified by the Division, SAPTA (Substance Abuse Prevention and Treatment Agency).
US Department of Agriculture
Information on opioid misuse in rural America and funding opportunities to address the misuse.
National Institute of Drug Abuse (NIDA)
Information on how drugs affect the brain and body for teens, teachers, and parents.
Prescribe 365
The Prescribe 365 website offers resources and information for opioid prescribers in Nevada.
Substance Abuse and Mental Health Services Administration (SAMHSA)
SAMHSA offers a wealth of resources for practitioners, including treatment guidelines, training materials, and publications specific to opioid use disorder. Their website provides access to evidence-based practices, treatment guidelines, and clinical tools.
Tools & Resources
The Conversation Guide for Delivering a Trauma-Informed Brief Intervention
The link between childhood trauma and substance use disorders is well-documented in the literature. This resource acknowledges that link and is intended to help healthcare providers deliver a brief intervention for substance use using a trauma-informed care approach. Whether you are well-versed in the Screening, Brief Intervention, and Referral to Treatment (SBIRT) process, or just looking for an effective way to address substance use concerns with your patients, this guide provides practical examples to facilitate that conversation. The left column provides scripts and concrete strategies to move through the brief intervention process, while the right column provides considerations to ensure trauma-informed care principles are integrated into the delivery.
Medications for Addiction Treatment (MAT) Resource Library
The MAT Resource Library is supported by the Los Angeles County Health Agency and Department of Public Health, Substance Abuse Prevention and Control. The site provides practical information on Medications for Addiction Treatment (MAT) for providers across health systems (e.g., physical health, mental health, and substance use disorder systems), as well as for patients.
Nevada Fentanyl Test Strip Distribution Sites
A list and map of Fentanyl Test Strip Distribution Sites in Nevada.
Nevada Overdose Reversal Medication Finder
Find naloxone and overdose reversal medications in Nevada.
Behavioral Health Nevada
This website is a database of behavioral health providers in Nevada specializing in substance use disorder and co-occurring mental health disorder treatment services. All agencies listed are Certified by the Division, SAPTA (Substance Abuse Prevention and Treatment Agency).
How to Use Fentanyl Test Strips
Infographics and step-by-step instructions.
Wound Care & Medical Triage for People Who Use Drugs and the Programs That Serve Them
This comprehensive guide provides information and recommendations regarding general health, safer use practices, common viral, fungal, parasitic, and other injection-related infections, overdose and overamp, tapering, withdrawal, medications for opioid use disorder, and seeking medical care.
Establishing Peer Support Services for Overdose Response: A Toolkit for Health Departments
Peer support services (PSS) are a valuable component of a growing number of overdose response and linkage to care initiatives that can be implemented and supported by local and state health departments. This toolkit is for local and state health departments and community partners who are exploring opportunities to implement or enhance PSS within overdose response and linkage to care initiatives. This toolkit provides information, resources, tools, actionable steps and real-world examples informed by the latest research, subject matter experts and experiences from diverse settings across the country.
Tools for Overdose Prevention
To help public health practitioners prevent overdose, the National Council for Mental Wellbeing, in partnership with the Centers for Disease Control and Prevention, developed these resources and tools for overdose prevention.
Screening Tools
Overdose Reversal Medication for Professionals
A Nevada provider's guide to prescribing Naloxone to patients who use opioids.
Opioid-Overdose Reduction Continuum of Care Approach (ORCCA) Practice Guide 2023
This guide was drawn from HEALing Communities Study (HCS) learnings to-date and expert insights to provide guidance regarding implementation of ORCCA menu strategies.
The Nevada Opioid Overdose Surveillance Dashboard
Includes graphs and tables on death rates, opioid-related emergency department visits and inpatient admissions, and opioid prescriptions at the county-level and zip code-level.
CDC Fatal Overdose (SUDORS) Dashboard
A dashboard to look at overdose death data for 2020 by substance for 29 states/jurisdictions.
CDC Non-Fatal Drug Overdose (DOSE) Dashboard
A dashboard to look at emergency department non-fatal overdose data since February 2018 for all drugs, all opioids, heroin, or all stimulants by state.
Medication for Opioid Use Disorder (MOUD) Tool Kit for Peer Recovery Specialists
This toolkit is a resource for Peer Recovery Specialists (PRSs) to feel equipped to discuss MOUD with providers, people seeking recovery, and others with questions about this treatment option.
Overdose Prevention and Response Toolkit
This toolkit provides guidance to a wide range of individuals on preventing and responding to an overdose. The toolkit also emphasizes that harm reduction and access to treatment are essential aspects of overdose prevention.
Storage and Disposal of Medication
Improper prescription drug use is a serious public health issue. Storing and disposing of medications properly can help reduce harm.
Posters & Infographics
Prescribe 365 Brochure
This brochure is for providers to print and display in their offices encouraging patients to openly discuss safe use of opioids.
Download Brochure
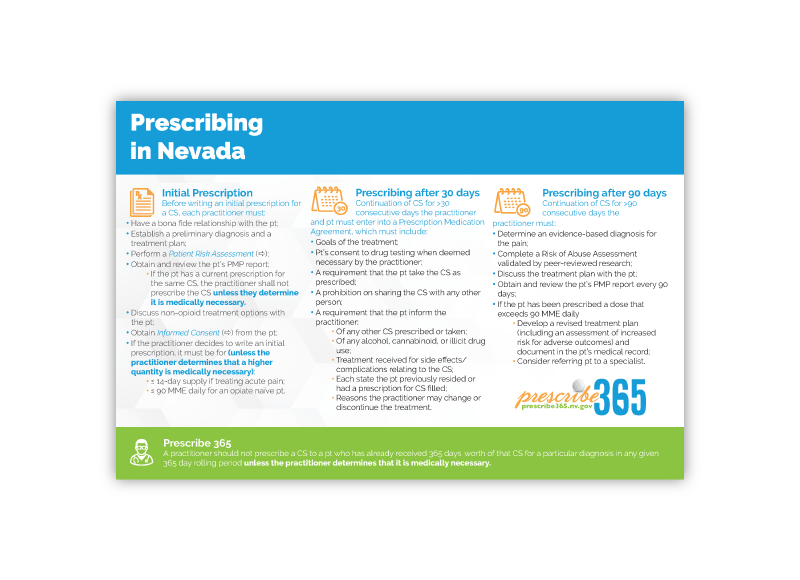
Prescribe 365 Prescribing in Nevada Pocket Card
The Prescribe 365 pocket card is intended for providers to print and display in their offices encouraging patients to openly discuss safe use of opioids.
Download Card
Prescribe 365 Prescribing in Nevada Pocket Card
The Prescribe 365 pocket card is intended for providers to print and display in their offices encouraging patients to openly discuss safe use of opioids.
Download the Pocket Card

Opioid Trifold Brochures
Opioid Information Brochures for Providers or Consumers help educate on opioids and opioid use, including effects of opioid use, pregnancy and opioid use, medications for opioid use including opioid overdose reversal medications, and treatment options for persons using opioids.
Download or request free hard copies

Stimulant Trifold Brochures
Stimulant Information Brochures for Providers or Consumers help educate on stimulants, including the effects of stimulants use, pregnancy and stimulant use, and treatment options for persons using stimulants.
Download or request free hard copies
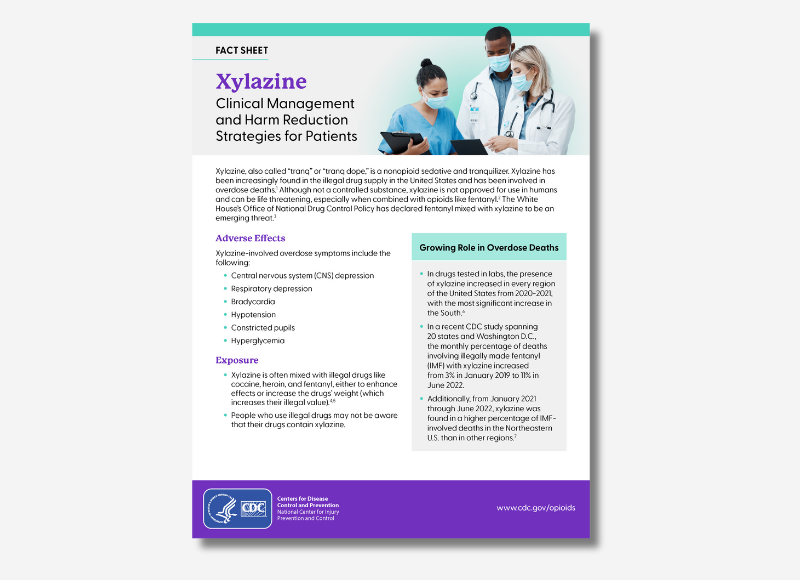
Xylazine: Clinical Management and Harm Reduction Strategies for Patients
This fact sheet is intended to guide healthcare professionals on the clinical management of Xylazine use and harm reduction strategies for their patients.
Download the fact sheet

Prevent Addiction Fact Sheet
This face sheet contains information for patients about preventing opioid addiction.
Download the fact sheet.
Publications
Alcohol Screening and Brief Intervention for Youth: A Practitioner’s Guide
“Alcohol Screening and Brief Intervention for Youth: A Practitioner’s Guide” is designed to help health care professionals quickly identify youth at risk for alcohol-related problems. NIAAA developed the Guide and Pocket Guide in collaboration with a team of underage drinking researchers and clinical specialists and practicing health care professionals.
Reducing the Stigma of Addiction: What we say and do matters to patients with substance use disorder
Johns Hopkins Medicine. (2024). Reducing the Stigma of Addiction. [Webpage]. Retrieved from [https://www.hopkinsmedicine.org/stigma-of-addiction]
Fast Facts About Substance Use Disorders: What Every Nurse, APRN, and PA Needs to Know (Book)
This resource is the first to provide evidence-based information and strategies for APRNs and PAs who work with individuals with substance use disorders (SUDs). Written in a concise, bulleted style for easy access to critical information, the reference addresses often-undiagnosed medical and psychiatric conditions which may accompany SUDs and the ethical considerations of working with affected patients and families.
Xylazine Basics: Overdose Prevention, Harm Reduction, and Wound Care
This document provides information on xylazine, a non-opioid veterinary tranquilizer used as an additive in illicit drug supplies, notably in combination with heroin and fentanyl. It discusses the effects of xylazine use, including sedation and potential risks such as hypotension and bradycardia. The document also emphasizes harm reduction interventions for individuals who may encounter xylazine in the drug supply, including the use of naloxone for responding to overdoses and the importance of wound identification and treatment.
Dear Colleague Letter – Xylazine
This "Dear Colleague" letter from the Substance Abuse and Mental Health Services Administration (SAMHSA) provides a report on the risks of Xylazine.
Opioid Use and Opioid Use Disorder in Pregnancy: A Joint Opinion of the ACOG’s Committee on Obstetric Practice and ASAM
The Society of Maternal–Fetal Medicine endorses this document. This Committee Opinion was developed by the American College of Obstetricians and Gynecologists’ Committee on Obstetric Practice in collaboration with committee members Maria A. Mascola, MD, MPH; Ann E. Borders, MD, MSc, MPH; and the American Society of Addiction Medicine member Mishka Terplan, MD, MPH.
Beyond Addiction: How Science and Kindness Help People Change
The most innovative leaders in progressive addiction treatment in the US offer a groundbreaking, science-based guide to helping loved ones overcome addiction problems and compulsive behaviors.
Opioid Use Disorder
This activity focuses on the critical evaluation and management of opioid use disorder (OUD), a pervasive condition significantly diminishing patients' quality of life and contributing to a widespread epidemic in the United States.
Webinars & Online Learning
Current News & Research
DEA Reports Widespread Threat of Fentanyl Mixed with Xylazine
WASHINGTON - The U.S. Drug Enforcement Administration is warning the American public of a sharp increase in the trafficking of fentanyl mixed with xylazine. Xylazine, also known as “Tranq,” is a powerful sedative that the U.S. Food and Drug Administration has approved for veterinary use.
Southern Nevada Health District calls attention to xylazine risk
The Southern Nevada Health District (SNHD) is urging heightened public awareness of the health dangers associated with xylazine, an animal tranquilizer that is increasingly being found in the country’s illicit drug supply and linked to overdose deaths throughout the United States. Xylazine, also known as “tranq,” is not approved for human consumption. It can be life-threatening and is especially dangerous when combined with opioids such as fentanyl.
Opioid Use Disorder Assessment Tools and Drug Screening
Opioid use disorder risk assessment tools cannot be used in isolation. In combination with standardized clinical examination, and, when indicated, urine drug screening, a validated risk assessment tool, improves the ability to detect opioid misuse. Even though no single tool has been shown to have both high interobserver reliability and high sensitivity, the standardized approach has still been shown to be superior to subjective care giver assessment. This article will provide a global approach to risk assessment in addition to reviewing the available tools.
The Opioid Epidemic’s Toll on Children
This article from the Johns Hopkins Bloomberg School of Public Health discusses the opioid epidemics toll on children.
“It’s called overamping”: experiences of overdose among people who use methamphetamine” by University of Nevada, Reno, School of Public Health & University of New Mexico Health Sciences
The USA is experiencing increases in methamphetamine use and methamphetamine-related or attributed deaths. In the current study, we explore qualitative narratives of methamphetamine overdose and strategies used by people who use drugs to reduce the undesirable effects associated with methamphetamine use.
Factors Associated With Calling 911 for an Overdose: An Ethnographic Decision Tree Modeling Approach
Between February 2017 and May 2018, we conducted qualitative interviews with 45 PWUDs who had seen an overdose, recruited from San Diego County, California, using outreach, referrals, and flyers...
Identification of Non-Fatal Opioid Overdose Cases Using 9-1-1 Computer Assisted Dispatch and Prehospital Patient Clinical Record Variables
he current epidemic of opioid overdoses in the United States necessitates a robust public health and clinical response. We described patterns of non-fatal opioid overdoses (NFOODs) in a small western region using data from the 9-1-1 Computer Assisted Dispatch (CAD) record and electronic Patient Clinical Records (ePCR) completed by EMS responders. ...
Filter Magazine – Why New 12-Step Members May Avoid Carrying Naloxone by Jeanette Bowles, PhD, University of California San Diego, Division of Infectious Diseases and Global Public Health
For new members of 12-step programs like Alcoholics Anonymous and Narcotics Anonymous, naloxone can still seem like a symbol of drug use, according to new research. This can cause some people looking to kick drugs through these large abstinence-based fellowships—NA, for example, holds 70,000 weekly meetings in 144 countries, according to a 2018 survey—to decline to carry the overdose-reversal drug, seeing it as a relic of a past life.
