Medications for Opioid Use Disorder (MOUD) is an umbrella term for medications used in the treatment of opioid addiction or opioid use disorder (OUD). These medications are typically prescribed as part of a comprehensive treatment program that also includes counseling and behavioral therapies.
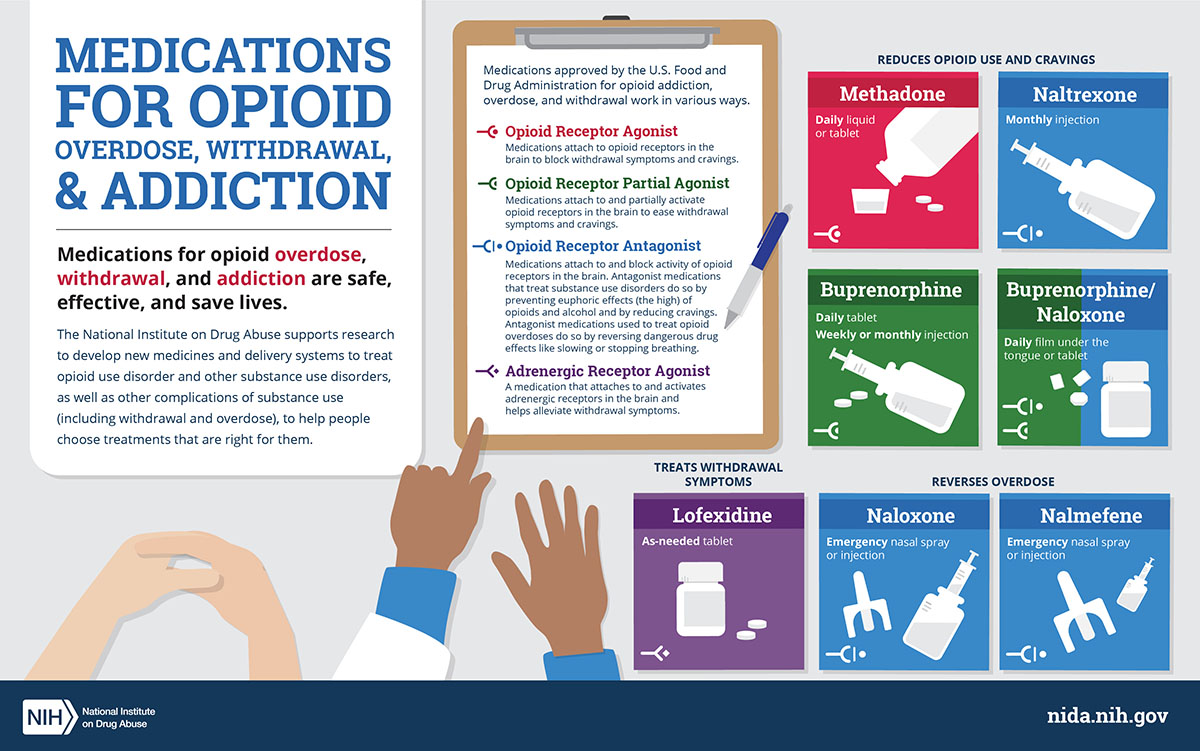
There are three main types of medications used in MOUD:
Methadone: Methadone is a long-acting opioid agonist. It works by binding to the same receptors in the brain as opioids, such as heroin or prescription painkillers, but it does so in a way that helps to reduce cravings and withdrawal symptoms without producing the same euphoric effects. Methadone is usually dispensed in specialized clinics on a daily basis.
Buprenorphine: Buprenorphine is a partial opioid agonist, meaning it also binds to opioid receptors but produces weaker effects compared to full opioid agonists like heroin or methadone. Buprenorphine helps to reduce cravings and withdrawal symptoms while also blocking the effects of other opioids, which can help prevent relapse. It is often prescribed in the form of sublingual tablets or films and can be administered in a doctor’s office.
Naltrexone: Naltrexone is an opioid antagonist, meaning it blocks the effects of opioids by binding to the same receptors in the brain without activating them. Unlike methadone and buprenorphine, which help to reduce cravings and withdrawal symptoms, naltrexone works by preventing opioids from producing any effects if they are taken. It is available in both oral and injectable forms.
Medications for Opioid Use Disorder (MOUD) Resources
Websites
Tools & Resources
Medications for Addiction Treatment (MAT) Resource Library
Medication-Assisted Treatment (MAT) for Opioid Use Disorder in Jails and Prisons: A Planning and Implementation Toolkit
Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
Medication-Assisted Treatment (MAT) for Opioid Use Disorder
Medication for Opioid Use Disorder (MOUD) Tool Kit for Peer Recovery Specialists
Publications
Decisions in Recovery: Treatment for Opioid Use Disorders
Medication-Assisted Treatment (MAT) Services for Opioid Dependence Billing Instructions Guide
Pocket Guide: Medication-Assisted Treatment of Opioid Use Disorders
TIP 63: Medications for Opioid Use Disorder
The Patient-Centered Opioid Addiction Treatment (P-COAT) Model
Posters & Infographics

Opioid Trifold Brochures