Opioid related overdose deaths have continued to increase following the introduction of fentanyl into the national drug supply and the increased isolation that resulted from the COVID-19 pandemic. Evidence-based and research-informed prevention activities have been found to be effective in overdose prevention by increasing accessibility to treatment services, improving the navigation of systems of care, engagement in early intervention, and practicing harm reduction strategies.
Websites
Good Samaritan Drug Overdose Act of 2015
The Good Samaritan Drug Overdose Act of 2015 (Senate Bill 459, Chapter 26, Statutes of Nevada 2015 NRS 453C.120) created various provisions addressing the opiate overdose epidemic that continues to claim over 300 lives per year in Nevada. The law prevents punitive actions against health professionals and any person who administers naloxone or calls 911 to assist someone who may be overdosing on opiates. It also provides immunity to persons seeking medical treatment for an opioid overdose for themselves or someone else. Learn more about the Good Samaritan Law.
Stop Overdose
To address the increasing number of overdose deaths related to both prescription opioids and illicit drugs, the Centers for Disease Control and Prevention (CDC) created a website to educate people who use drugs about the dangers of illicitly manufactured fentanyl, the risks and consequences of mixing drugs, the lifesaving power of naloxone, and the importance of reducing stigma around recovery and treatment options.
Tools & Resources
Opioid Epidemic Response: Employer Toolkit
Substance use and substance use disorder affects employees, workplaces, families, and communities. Employers have the opportunity to identify early signs and symptoms of a substance use disorder, and help connect employees to treatment and recovery supports. This toolkit developed by the Minnesota Department of Health includes five steps to prevent and address substance use disorder within your workplace.
International Overdose Awareness Day
International Overdose Awareness Day spreads the message about the tragedy of drug overdose death and that drug overdose is preventable.
The Opioid Guide: A Resource Guide for Practicing Psychologists
A guide from the American Psychological Society with information for practicing psychologists on opioids, their use, and effective treatments.
Wound Care & Medical Triage for People Who Use Drugs and the Programs That Serve Them
This comprehensive guide provides information and recommendations regarding general health, safer use practices, common viral, fungal, parasitic, and other injection-related infections, overdose and overamp, tapering, withdrawal, medications for opioid use disorder, and seeking medical care.
Establishing Peer Support Services for Overdose Response: A Toolkit for Health Departments
Peer support services (PSS) are a valuable component of a growing number of overdose response and linkage to care initiatives that can be implemented and supported by local and state health departments. This toolkit is for local and state health departments and community partners who are exploring opportunities to implement or enhance PSS within overdose response and linkage to care initiatives. This toolkit provides information, resources, tools, actionable steps and real-world examples informed by the latest research, subject matter experts and experiences from diverse settings across the country.
Tools for Overdose Prevention
To help public health practitioners prevent overdose, the National Council for Mental Wellbeing, in partnership with the Centers for Disease Control and Prevention, developed these resources and tools for overdose prevention.
Never Use Alone
Toll-free national overdose prevention, detection, life-saving crisis response and medical intervention services for people who use drugs while alone. Never Use Alone’s peer operators are available 24-hours a day, 7 days a week, 365 days a year.
Overdose Reversal Medication for Individuals & Families
Guides to opioid safety and how to use overdose reversal medications.
Engaging Community Coalitions to Decrease Opioid Overdose Deaths Practice Guide 2023
This guide was developed in recognition of the need to center community engagement throughout the efforts to address the opioid overdose crisis. This guide exists to help communities decrease opioid overdose deaths; it includes tools and real-world examples that can be used to build and strengthen community coalitions that work to reduce opioid overdose deaths.
Overdose Reversal Medication for Community Organizations
This guide includes Naloxone Distribution in Nevada guidelines and best practices for community based organizations.
Overdose Reversal Medication for Professionals
A Nevada provider's guide to prescribing Naloxone to patients who use opioids.
Opioid-Overdose Reduction Continuum of Care Approach (ORCCA) Practice Guide 2023
This guide was drawn from HEALing Communities Study (HCS) learnings to-date and expert insights to provide guidance regarding implementation of ORCCA menu strategies.
Overdose Prevention and Response Toolkit
This toolkit provides guidance to a wide range of individuals on preventing and responding to an overdose. The toolkit also emphasizes that harm reduction and access to treatment are essential aspects of overdose prevention.
Publications
Good Samaritan Fatal Overdose Prevention and Drug-induced Homicide: Summary of State Laws
Research indicates that there is often a reluctance among those witnessing an overdose to summon emergency assistance from law enforcement or other first responders out of fear of arrest for drug possession or other charges. In an effort to reduce this fear and to encourage overdose witnesses to seek help, state policymakers developed Good Samaritan laws specific to drug overdoses. The purpose of these laws is to prioritize the overdose victim’s safety over arresting drug users by granting limited protection from criminal liability to persons seeking medical assistance and, in most cases, to the overdose victim. This document (1) provides a singular resource for each jurisdiction’s laws; (2) allows for a comparison of these laws between jurisdictions; and (3) identifies and highlights interesting provisions.
Xylazine Basics: Overdose Prevention, Harm Reduction, and Wound Care
This document provides information on xylazine, a non-opioid veterinary tranquilizer used as an additive in illicit drug supplies, notably in combination with heroin and fentanyl. It discusses the effects of xylazine use, including sedation and potential risks such as hypotension and bradycardia. The document also emphasizes harm reduction interventions for individuals who may encounter xylazine in the drug supply, including the use of naloxone for responding to overdoses and the importance of wound identification and treatment.
Evidence-Based Strategies for Preventing Opioid Overdose: What’s Working in the United States
There are strategies that can assist community leaders, local and regional organizers, non-profit groups, law enforcement, public health, and members of the public in understanding and navigating effective ways to prevent opioid overdose in their communities. Use this information as a reference for evidence-based practices that have been successfully implemented in the U.S.
Heroin, Fentanyl, & Other Opioids: A Comprehensive Resource for Families with a Teen or Young Adult Struggling with Opioid Use
Fueled by drugs like heroin, fentanyl and the misuse of prescription pain pills, the opioid epidemic in our country has impacted countless families. To help address this, the Partnership for Drug-Free Kids created a new eBook — Heroin, Fentanyl & Other Opioids: A Comprehensive Resource for Families with a Teen or Young Adult Struggling with Opioid Use. Parents and families need to be prepared with the knowledge and skills to identify opioids, spot early use and take action effectively.
Posters & Infographics
Be Prepared – (Poster)
This poster illustrates being prepared for an overdose emergency by having an opioid overdose reversal medication on-hand, just like people commonly have a fire extinguisher on-hand for a fire emergency.
Download or request hard copies

Opioid Trifold Brochures
Opioid Information Brochures for Providers or Consumers help educate on opioids and opioid use, including effects of opioid use, pregnancy and opioid use, medications for opioid use including opioid overdose reversal medications, and treatment options for persons using opioids.
Download or request free hard copies
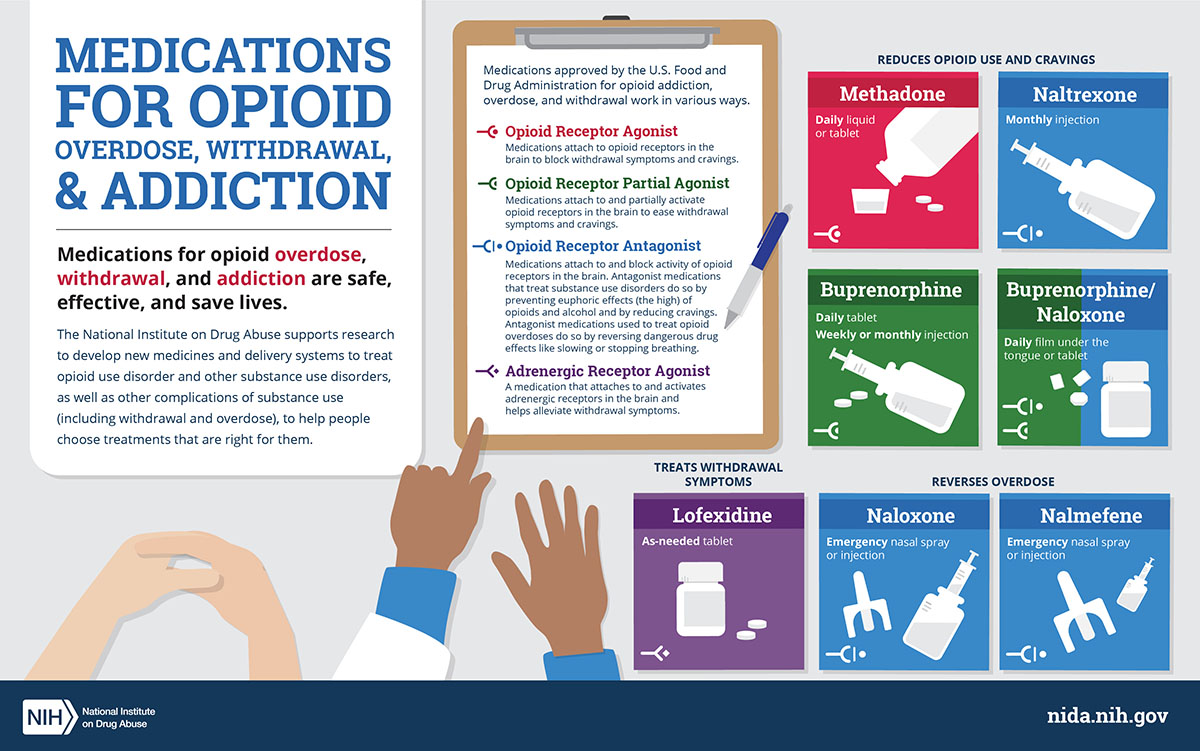
Medications for Opioid Use Disorder (MOUD) Infographic
This infographic shows different types of medications approved by the U.S. Food and Drug Administration for opioid overdose, withdrawal, and addiction.
Download the infographic
Webinars & Online Learning
Current News & Research
The Mobile Emergency Recovery Intervention Trial (MERIT)
The Mobile Emergency Recovery Intervention Trial (MERIT) is a grant-funded research study that is evaluating the effectiveness and long-term outcomes of an ER-based intervention for opioid overdose patients treated in Nevada’s Emergency Departments (EDs). The research is currently ongoing.
