Stimulant use disorder (StimUD) is a substance use disorder involving any of the class of drugs that include cocaine, methamphetamine, and prescription stimulants. Stimulant use is increasing the United States. According to the most recent data available from the National Survey on Drug Use and Health (NSDUH), in 2020, an estimated 5.1 million people aged 12 or older misused prescription stimulants in the past year. Young adults aged 18 to 25 had the highest percentage of prescription stimulant misuse in the past year. Approximately 2.6 million people aged 12 or older used methamphetamine in the past year, an increase of over 36% from 2018. 1.8 million people aged 12 or older used cocaine in the past year, which represented a significant decrease from 2018.
Stimulant Use Disorder Resources
Websites
Get the facts on Stimulant Use Disorder
U.S. Department of Veterans Affairs: Stimulant Use Disorder
Stimulant Abuse: Signs, Effects, and Treatment Options
Good Samaritan Drug Overdose Act of 2015
Tools & Resources
SAMHSA’s TIP 33: Treatment for Stimulant Use Disorders
SAMHSA’s Evidence-Based Resource Guide Series: Treatment of Stimulant Use Disorders
The ASAM/AAAP Clinical Practice Guideline on the Management of Stimulant Use Disorder
Centers for Disease Control and Prevention (CDC) Stimulant Guide
Publications
Fast Facts About Substance Use Disorders: What Every Nurse, APRN, and PA Needs to Know (Book)
Current Diagnosis & Treatment: Psychiatry, 3e: Chapter 51: Stimulant Use Disorders
Psychiatric Annals: Stimulant Use Disorders
Frontline: Meth and the Brain
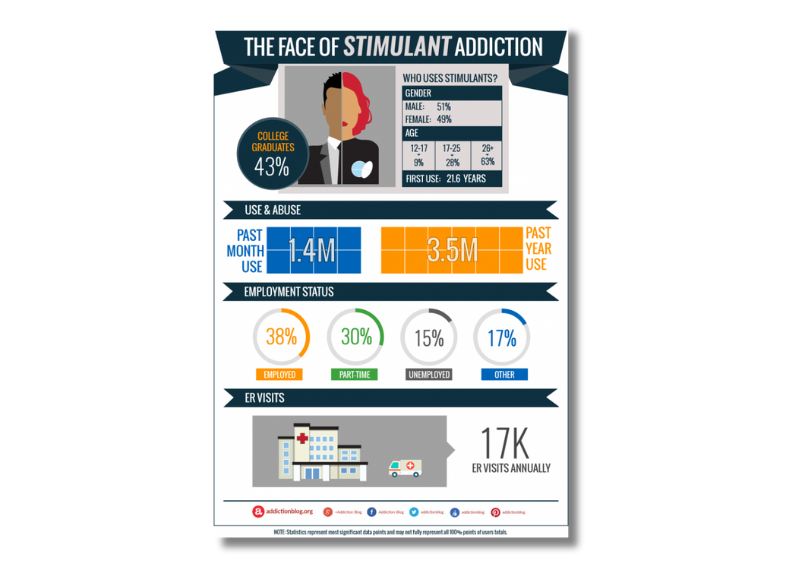
Posters & Infographics

Stimulant Trifold Brochures
![What are Stimulants? Stimulants speed up the body’s systems. This class of drugs includes: Prescription drugs such as amphetamines [Adder- all® and Dexedrine®], methylphenidate [Concerta® and Ritalin®], diet aids [such as Didrex®, Bontril®, Preludin®, Fastin®, Adipex P®, Ionomin®, and Meridia®] and other illicitly used drugs such as methamphetamine, cocaine, methcathinone, and other synthetic cathinones that are commonly sold under the guise of “bath salts.” Street Title Bennies, Black Beauties, Cat, Coke, Crank, Crystal, Flake, Ice, Pellets, R-Ball, Skippy, Snow, Speed, Uppers, Vitamin R How are they abused? Stimulants can be pills or capsules that are swallowed. Smoking, snorting, or injecting stimulants produces a sudden sensation known as a “rush” or a “flash. Abuse is often associated with a pattern of binge use - sporadically consuming large doses of stimulants over a short period of time. Heavy users may inject themselves every few hours, continuing until they have depleted their drug supply or reached a point of delirium, psychosis, and physical exhaustion.During heavy use, all other interests become secondary to recreating the initial euphoric rush. What is their effect on the body? Stimulants are sometimes referred to as uppers and reverse the effects of fatigue on both mental and physical tasks. Therapeutic levels of stimulants can produce exhilaration, extended wakefulness, and loss of appetite. These effects are greatly intensified when large doses of stimulants are taken. Taking too large a dose at one time or taking large doses over an extended period of time may cause such physical side effects as: Dizziness, tremors, headache, flushed skin, chest pain with palpitations, excessive sweating, vomiting, and abdominal cramps. When used as drugs of abuse and not under a doctor’s supervision, stimulants are frequently taken to: Produce a sense of exhilaration, enhance self-esteem, improve mental and physical performance, increase activity, reduce appetite, extend wakefulness for prolonged period, and “get high”. Chronic, high-dose use is frequently associated with agitation, hostility, panic, aggression, and suicidal or homicidal tendencies.Paranoia, sometimes accompanied by both auditory and visual hallucinations, may also occur. What are their overdose effects? In overdose, unless there is medical intervention, high fever, convulsions, and cardiovascular collapse may precede death. Because accidental death is partially due to the effects of stimulants on the body’s cardiovascular and temperature- regulating systems, physical exertion increases the hazards of stimulant use.](https://nvopioidresponse.org/wp-content/uploads/2024/04/NOCE-Infographic-Resource-4.png)
Drug Fact Sheet: Stimulants