Xylazine, commonly referred to as tranq or tranq dope, is an animal tranquilizer that is increasingly found in the illicit drug supply. Xylazine can result in life-threatening outcomes, especially when combined with opioid use. This use of Xylazine in conjunction with opioids has been declared an emerging threat by the White House’s Office of National Drug Control Policy and has been appearing more frequently throughout the United States.
Common symptoms of Xylazine use include (FDA):
- Sedation.
- Difficulty breathing.
- Dangerously low blood pressure.
- Slowed heart rate.
- Wounds that can become infected.
- Severe withdrawal symptoms.
- Death.
Response to a possible overdose involving Xylazine:
- Call 911
- Initiate rescue breathing or chest compressions. This ensures that the individual is receiving oxygen. Rescue breathing has been found especially beneficial for those in an overdose state as the respiratory system is compromised by the substance.
- Administer naloxone. Naloxone can reverse the effect of opioids that may be in the system and contributing to the overdose state. It will not reverse the effect of Xylazine. Rescue breathing or chest compressions may need to be continued.
Websites
Good Samaritan Drug Overdose Act of 2015
The Good Samaritan Drug Overdose Act of 2015 (Senate Bill 459, Chapter 26, Statutes of Nevada 2015 NRS 453C.120) created various provisions addressing the opiate overdose epidemic that continues to claim over 300 lives per year in Nevada. The law prevents punitive actions against health professionals and any person who administers naloxone or calls 911 to assist someone who may be overdosing on opiates. It also provides immunity to persons seeking medical treatment for an opioid overdose for themselves or someone else. Learn more about the Good Samaritan Law.
What is Xylazine?
Information about Xylazine, commonly referred to as tranq or tranq dope, an animal tranquilizer that is increasingly found in the illicit drug supply.
Tools & Resources
Wound Care & Medical Triage for People Who Use Drugs and the Programs That Serve Them
This comprehensive guide provides information and recommendations regarding general health, safer use practices, common viral, fungal, parasitic, and other injection-related infections, overdose and overamp, tapering, withdrawal, medications for opioid use disorder, and seeking medical care.
Never Use Alone
Toll-free national overdose prevention, detection, life-saving crisis response and medical intervention services for people who use drugs while alone. Never Use Alone’s peer operators are available 24-hours a day, 7 days a week, 365 days a year.
Publications
Xylazine Basics: Overdose Prevention, Harm Reduction, and Wound Care
This document provides information on xylazine, a non-opioid veterinary tranquilizer used as an additive in illicit drug supplies, notably in combination with heroin and fentanyl. It discusses the effects of xylazine use, including sedation and potential risks such as hypotension and bradycardia. The document also emphasizes harm reduction interventions for individuals who may encounter xylazine in the drug supply, including the use of naloxone for responding to overdoses and the importance of wound identification and treatment.
Dear Colleague Letter – Xylazine
This "Dear Colleague" letter from the Substance Abuse and Mental Health Services Administration (SAMHSA) provides a report on the risks of Xylazine.
Posters & Infographics
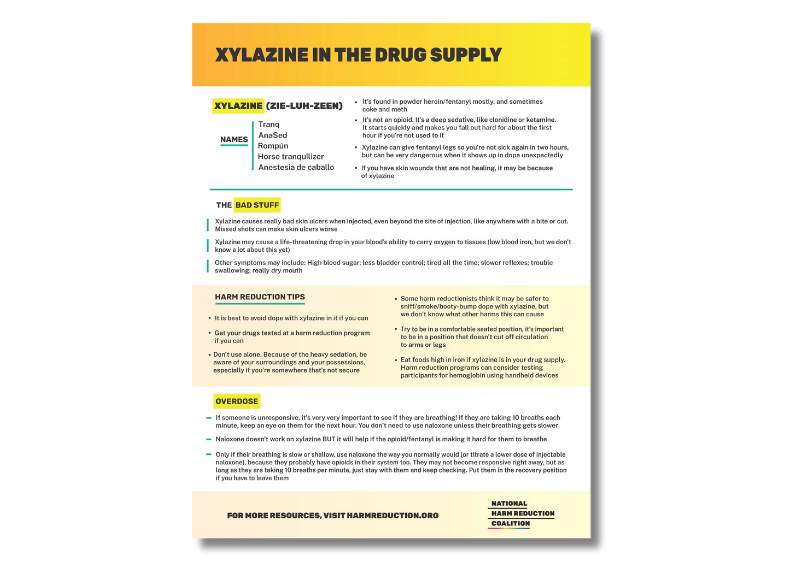
Xylazine in the Drug Supply Infographic
This infographic from the National Harm Reduction Coalition contains information on Xylazine in the drug supply.
Download the infographic
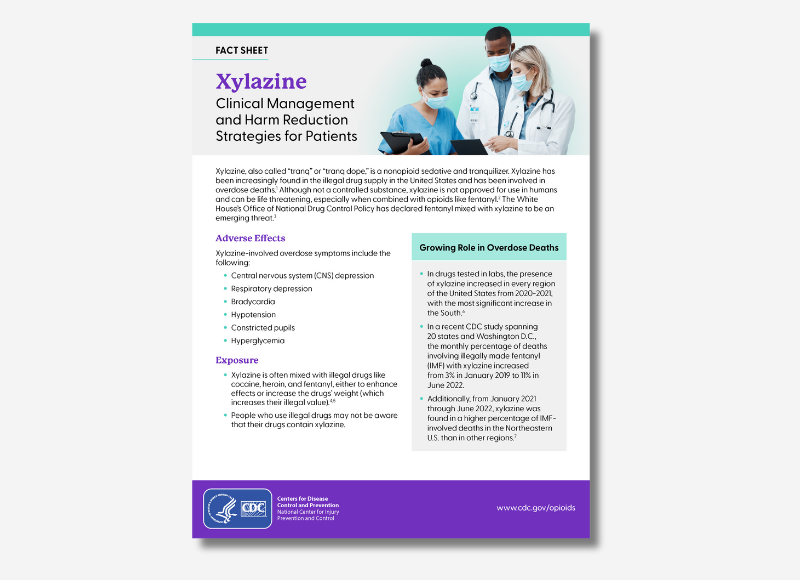
Xylazine: Clinical Management and Harm Reduction Strategies for Patients
This fact sheet is intended to guide healthcare professionals on the clinical management of Xylazine use and harm reduction strategies for their patients.
Download the fact sheet
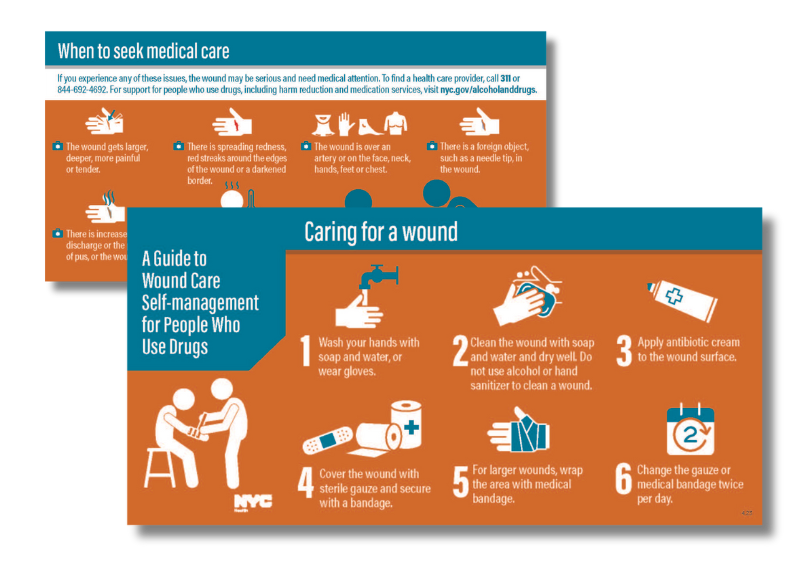
Wound Care Pocket Card
This pocket card from NYC.gov is a guide to wound care self-management for people who use drugs.
Download the Wound Care Pocket Card
Webinars & Online Learning
Current News & Research
DEA Reports Widespread Threat of Fentanyl Mixed with Xylazine
WASHINGTON - The U.S. Drug Enforcement Administration is warning the American public of a sharp increase in the trafficking of fentanyl mixed with xylazine. Xylazine, also known as “Tranq,” is a powerful sedative that the U.S. Food and Drug Administration has approved for veterinary use.
Southern Nevada Health District calls attention to xylazine risk
The Southern Nevada Health District (SNHD) is urging heightened public awareness of the health dangers associated with xylazine, an animal tranquilizer that is increasingly being found in the country’s illicit drug supply and linked to overdose deaths throughout the United States. Xylazine, also known as “tranq,” is not approved for human consumption. It can be life-threatening and is especially dangerous when combined with opioids such as fentanyl.
